Naloxone, a life-saving antidote to drug overdose: myths and facts
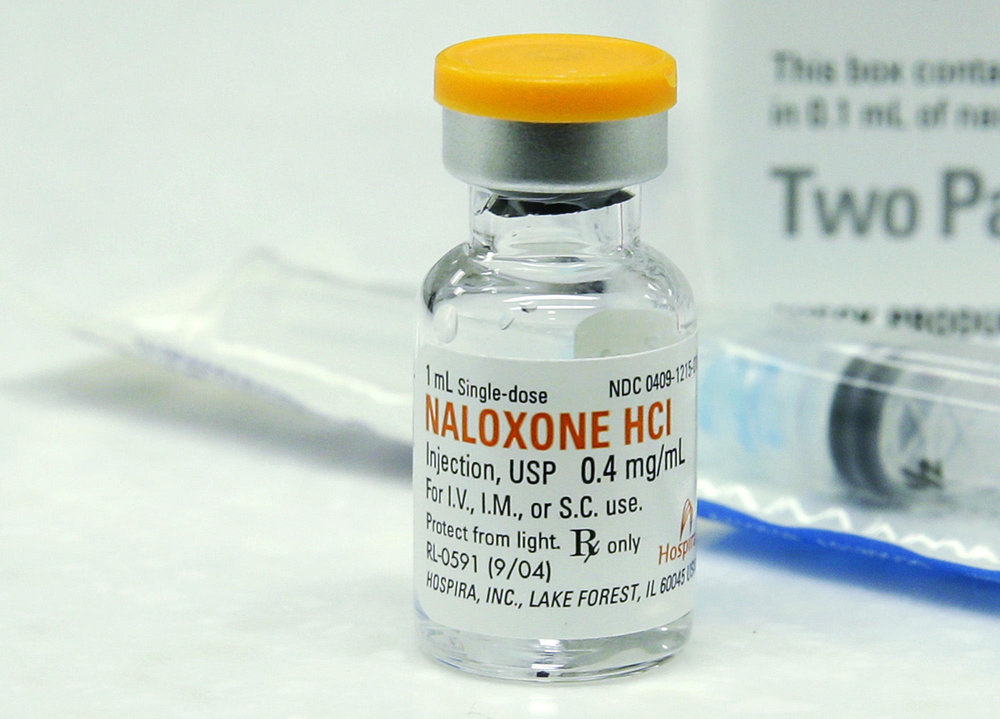
TEHRAN — According to World Health organization (WHO), Opioid overdose is treatable with naloxone, an opioid antagonist which rapidly reverses the effects of opioids.
In Iran, there are different opinions about the correct usage of naloxone.
Last week, the Food and Drug Administration’s spokesperson announced that self-injection or non-prescribed usage of naloxone could have catastrophic consequences, even leading to adverse side effects on the heart.
Kianoush Jahanpour added that naloxone should be used only under a physician’s supervision and with emergency room equipment, as it is usually used in emergency situations in hospitals.
Meanwhile, Health Ministry’s Spokesperson Iraj Harirchi said on Monday that according to Iran’s current laws, naloxone is only accessible in hospitals.
He said that naloxone is available in some countries in the format of nasal sprays or even edibles, but in Iran people should be first properly trained on this drug’s usage, before making it available in pharmacies, especially if parenteral route of administration is used.
In an interview with Khabaronline on Monday, Dr. Omran Mohammad Razaqi said that naloxone nasal sprays which are extremely easy to use aren’t available in Iran, but the drug can also be administrated intravenously by bystanders who can perform injections.
According to WHO, naloxone has been used in the management of opioid overdose for more than 40 years. It is a safe drug with a low risk of serious side effects and any adult capable of learning basic life support can also learn to recognize an opioid overdose, and administer naloxone in time to save lives.
Educating people on usage of naloxone
WHO has announced that globally, an estimated 69,000 people die each year from opioid overdose alone. Among people who inject drugs, opioid overdose is the second most common cause of death after HIV/AIDS.
On November 4, 2014, WHO published guidelines aimed to reduce the number of opioid-related deaths globally. The guidelines recommend countries expand naloxone access to people likely to witness an overdose in their community, such as friends, family members, partners of people who use drugs, and social workers.
Naloxone is usually used with basic life support which is generally only available in medical settings, however, the guidelines recommend that people who are likely to witness an opioid overdose should be given access to naloxone and training in its use.
Route of administration
WHO guidelines recognizes that naloxone is effective when delivered by intravenous, intramuscular, subcutaneous and intranasal routes of administration. Persons using naloxone should select a route of administration based on the formulation available, their skills in administration, the setting and local context.
A study on naloxone distribution and administration by peers in Australia found that 74% of interviewees preferred using the intranasal route of administration.
Calls for naloxone widespread adoption
In recent years, a number of programs around the world have shown that it is feasible to provide naloxone to people likely to witness an opioid overdose, in combination with training on the use of naloxone and the resuscitation of people experiencing opioid overdose, prompting calls for the widespread adoption of this approach.
In 2012, the United Nations Economic and Social Council (ECOSOC) called upon the World Health Organization (WHO), in collaboration with the United Nations Office on Drugs and Crime (UNODC) to provide advice and guidance, based on scientific evidence, on preventing mortality from drug overdose, in particular opioid overdose.
Access to naloxone
Access to naloxone is generally limited to health professionals, and in many countries there is limited availability of naloxone even in medical settings, including ambulances.
Naloxone is a prescription medicine in almost all countries, and while it is not usually prescribed to people likely to witness an opioid overdose, at least one country has made naloxone available in pharmacies without prescription.
Side effects
Naloxone has been used in opioid overdose management for over 40 years, with minimal adverse effects beyond the induction of opioid withdrawal symptoms. It carries no potential for abuse, although high doses may lead to the development of opioid withdrawal symptoms such as vomiting, muscle cramps and agitation.
Does naloxone only work for overdose cases caused by opioids?
The Iranian Food and Drug Administration’s Deputy Director said last week that naloxone does not reverse the effects of benzodiazepines and stimulants such as cocaine, crystal meth (Methamphetamine) and ecstasy.
According to naloxoneinfo.org, naloxone only reverses the effects of opioids such as heroin, methadone, morphine, opium, codeine, or hydrocodone. It does not counter the effect of other types of drugs, such as benzodiazepines (drugs including diazepam, midazolam, or alprazolam), antihistamines (like pheniramine or phenergan), alcohol, or other sedatives (drugs such as phenobarbital) or stimulants such as cocaine and amphetamines. But if the person is not breathing it will not hurt to administer naloxone.
In the worst case scenario, naloxone will simply do nothing, but in the best case scenario it will save a life.
Study suggests anti-overdose med naloxone increases reckless opioid use
In March, CNBC published a controversial new study arguing that laws expanding access to naloxone have increased opioid-related ER visits and theft while doing nothing to curb mortality.
The study found opioid-related deaths increased 14 percent in the Midwest after these laws were in effect.
The authors believe that people act more recklessly when they have a safeguard in place, but the study's findings could just be correlation instead of causation.
SJ/MQ/MG

Leave a Comment